If anyone ever mentioned, 30 years ago, that at one moment, approaching a health centre for HIV/Aids treatment, their dreams would be received by deaf ears.
However, 30 years later, HIV/Aids, despite its continued existence, is something patients have grown to live with and contain. Lately, Uganda’s HIV response has reached a new high point, with antiretroviral (ARV) medication more readily available than ever—ensuring life‐saving treatment is no longer a barrier but a beacon of hope.
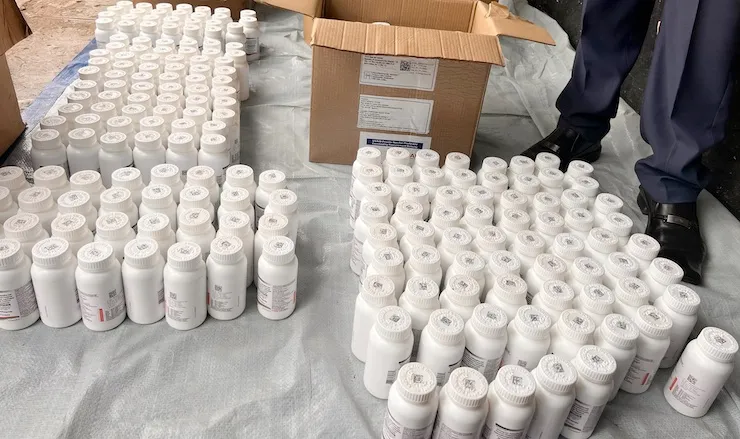
The ministry of Health, earlier this year, confirmed that ARVs remain fully stocked and freely distributed at all public and not‐ for‐profit health facilities across Uganda. National Medical Stores and Joint Medical Stores supply over 2,000 facilities bi-monthly, and no ARV stockouts have been reported in the past two years.
According to the ministry of Health, more than 1.4 million Ugandans are currently on ARV therapy, with viral suppression rates at an impressive 89%. Uganda Aids Commission adds, the country is nearing the global 95‐95‐95 targets, a milestone in the fight against HIV/Aids.
Perhaps one of the most profound changes has been cultural. Where stigma and secrecy once shadowed those on ARVs, today’s reality is far more empowering. Many people living with HIV now speak openly about their status and treatment, thanks to widespread awareness campaigns, media advocacy, and support from celebrities and community leaders.
“I take my medicine every day, and I have no reason to hide it,” says Leonard Mugume, a peer educator in Wakiso.
“There is no shame in staying alive and being healthy.” Community health programs have played a key role in shifting public attitudes, especially among youth and in urban areas, where taking ARVs is increasingly viewed as normal and responsible.
Social media platforms and radio talk shows have also opened space for open dialogue about HIV/Aids, helping erase fear and misinformation that once fueled discrimination. Even in schools, learners now receive age‐appropriate education about HIV and treatment adherence— further normalizing ARV use and reducing stigma.
In districts like Masaka, Kampala, and Wakiso, new community pharmacy distribution models are changing how people access medication. Through initiatives like those by Taso and the Infectious Disease Institute, stable patients can now collect their drugs at nearby pharmacies instead of queuing for hours at hospitals.
“I used to hide my pills like I was hiding a weapon. But now, I even remind my friends to take theirs. Things have really changed.” Says Rachael Namuleme (Not real name), a good vendor in Kireka
Additionally, differentiated service delivery (DSD) models—including multi-month dispensing and peer‐led groups— allow clients to receive refills every 3 to 6 months, improving privacy and convenience.